Diabetes UK is encouraging the use of technology to improve diabetes management and save the NHS vital funds. Nikki Joule, policy manager at Diabetes UK, puts the available technologies into context, explaining not only why they are important for helping people living with diabetes manage their condition as well as possible, but also why decision makers and budget holders should recognise the very real difference they can make to the NHS
Living with Type 1 or Type 2 diabetes is not easy. Managing the condition well requires vigilance, and 365-day-a-year management that can – in many cases – take a heavy toll on the physical and mental health and well-being of not only the person living with the condition, but also their families and those close to them.
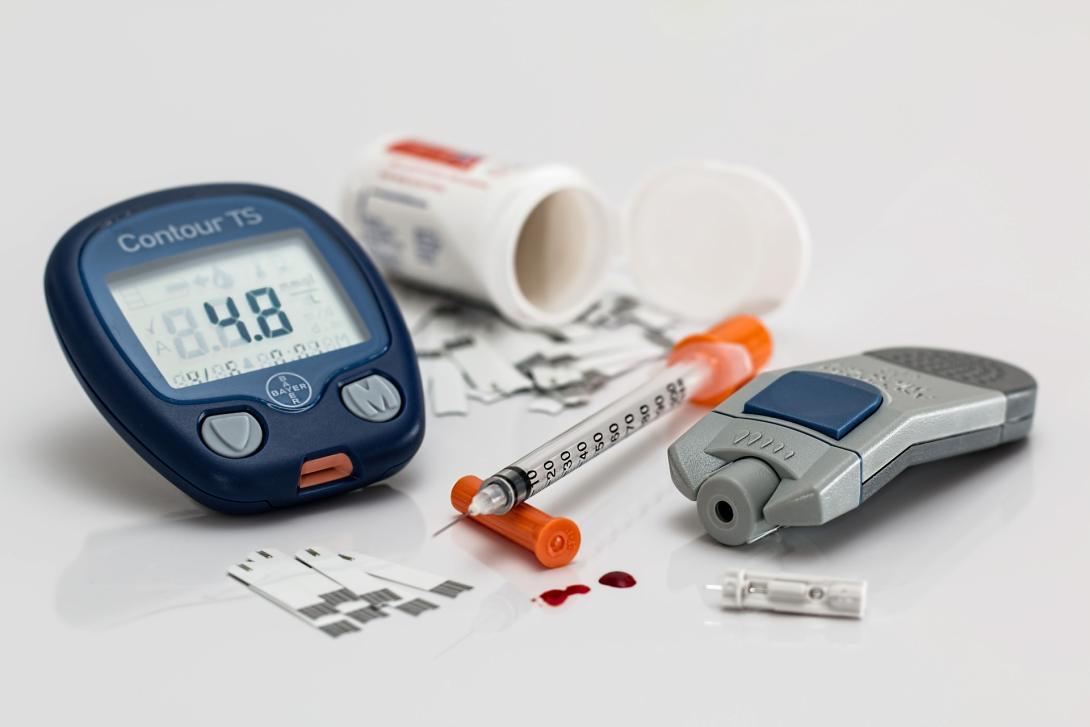
However, technologies designed to help manage the condition exist and, for those who are able to access them, they are making a significant difference to the lives of people living with diabetes. We know that technologies such as insulin pumps, continuous glucose monitors (CGM) and flash glucose monitoring (Flash GM) help people with Type 1 diabetes better manage their blood glucose, improving their quality of life overall and – equally important – reducing short term and long term complications.
Despite these clear benefits, the fact is that for too many people living with diabetes across the UK, access to these life-changing technologies remains a real issue, and variation in access means that people’s clinical needs are not being met, despite the obvious benefits that these technologies could have.
The NICE guidance for CGM and pumps is clear, but we know that many people, both children and adults, who meet this guidance are, for many reasons, still not able to take advantage of technology that would make managing their condition easier. Equally, despite being approved for prescription on the NHS late last year, many thousands of people who’d benefit from access to Flash GM are still either having to self-fund – at considerable personal cost – or simply go without.
An expensive condition
A large reason for this is cost. Diabetes is an expensive condition to treat; £10 billion a year is currently spent on diabetes, which represents around 10 per cent of the entire NHS budget. For newer technologies like Flash GM, dozens of Clinical Commissioning Groups (CCG’s) across England have decided they cannot afford to make it available because they simply cannot afford to do so.
The irony is that a significant chunk of this spend goes towards the treatment and management of the complications of diabetes that these technologies can actually help to prevent. Both the long and short term complications of diabetes are incredibly serious. In the short term this can mean extended periods of severe hypoglycaemia - and hyperglycaemia which can lead to hospital admission, missed days at work and loss of productivity. In the long term, however, the complications can be deadly; poor management of the condition can lead to heart disease, renal failure, amputations, blindness and even death.
In addition to fears concerning cost, the other reason for lack of, and variation in, access is awareness among clinicians about the benefits these technologies can have on both the daily quality of life, and the reduced risk of complications. Frustratingly, in other parts of Europe, we’re seeing far more enthusiasm for these technologies, and far less variation in access. In Germany we know there are significantly more people using pumps and CGM technology, while in France, for example, we also know that there is notably broader access to Flash GM.
Diabetes technology
To challenge this, Diabetes UK is working with NHS England, diabetes patient organisations JDRF and INPUT, and diabetes specialists to develop a diabetes technology pathway. This new consensus guidance, to be published later this year, will help inform clinicians about the use of technologies in the management of Type 1 diabetes, and will in turn help them consider these technologies when designing treatment and management support for people living with the condition.
Specifically in relation to Flash GM, in September of last year we published a consensus statement in partnership with JDRF, the Primary Care Diabetes Society, INPUT, the diabetes inpatient specialist nurses (DISN) group and the Association of British Clinical Diabetologists. In it, we outline our recommendations for the use of Flash GM, outlining the clinical evidence, what it offers to people with diabetes in terms of managing their condition, and the role healthcare professionals, and service funders and providers, can play in making this technology available.
Diabetes UK believes everyone with diabetes should have access to the right technology to support them, not just those who can afford it. That’s why we campaigned Flash Glucose Monitoring to be free on the NHS. However, nearly six months on, access to this life-changing technology is still very much a pipe dream for many thousands of people, while CCGs and health boards decide whether to fund Flash GM in their areas.
Ultimately, it is up to local health decision makers to create local policies so people can access these technologies. But Diabetes UK will continue campaigning, and raising awareness among healthcare professionals, decision makers and budget holders; the very clear benefits not only to the health and well-being of people living with diabetes, but also to the NHS budget, cannot be ignored.